Assignment 1: The Human Tongue
Function
The tongue is an organ that lies within the oral cavity in humans and many terrestrial vertebrates. The tongue is important in the functioning of multiple human processes and is very important in day to day life. Firstly, the tongue is one of the first organs which interact with food in the digestive tract. The tongue plays an important role in the process of mastication (chewing and grinding food) and begins the first step of digestion by breaking down some lipids [11]. The tongue pushes the food against teeth and the palate and aids in creating a bolus (ball) of food ready for further processing [5]. The muscular tissue is then used to send food from the oral cavity to the esophagus where it can proceed further into the digestive tract.
Although digestion is probably the main function of the tongue, it is used for many more processes by humans and animals. The main focus of this blog is on the tongue as a sensory organ. The tongue plays an extremely important role in sensing chemicals which are in the oral cavity [5]. This sense is known as Gustation. Gustation along with the olfactory sense (smell), produce a combined sense that we refer to as taste [5].
Other functions of the tongue are a result of its capability of fine motor movement. Changing the shape of the tongue can allow animals to produce different sounds and allow humans to communicate through language (by allowing fine phonetic pronunciations which results in articulated speech) [5]. Some sources also list the tongue as a key organ involved in intimacy and sexuality, and is actually part of the erogenous zone of the mouth [5].
Structure
The tongue is a very muscular tissue that resides in the oral cavity in humans. The tongue can be separated into various sections due to physical lines of connective tissue or lines that divide structure and function of the tongue. Firstly the tongue is separated into nearly symmetrical halves into left and right sections by a dividing line of fibrous connective tissue called the lingual septum [8]. This dividing line produces a groove called the median lingual sulcus, which is visible when looking at the tongue with the human eye.| Figure 1: Areas of the Tongue |
 |
| Figure 2: Sulcus Terminalis |
Development
 |
| Figure 3: Tongue Bud |
 |
| Figure 4: Pharyngeal Arch Development |
The frenulum is also an important tissue which forms and connects to the ventral surface of the tongue. During early development the lingual frenulum limits the movements of the fetal tongue to avoid damage. This function continues on until adulthood, but some issues may arise depending on how large the frenulum is. If the frenulum limits the movement of the tongue too much it leads to being tongue-tied (ankyloglossia), where impairments in speech and breast feeding may be seen [4].
| Figure 5: Frenulum of the Tongue |
Histology
The tongue is a primarily muscular tissue as the main function is to serve in mastication.The tongue has a highly convoluted epithelium, with associated taste buds and glandular tissue. The lamina propria of the tongue is seen to have dense, loose, and fibrous connective tissue as well as containing some adipose tissue [8].Oral Mucosa
 |
| Figure 6: Tissues covered by Oral Mucosa in the Oral Cavity |
| Figure 7: Surfaces of the tongue under a light microscope |
Papillae
 |
| Figure 8: Locations of Each type of Papillae |
| Figure 9: 4 Types of Papillae |
Glandular Tissue
The oral cavity produces many mucous and serous secretions which produce what is generally referred to as whole saliva [11]. The glands generally found in the oral cavity are mucous secreting, which contribute to the massive volume of saliva produced in a day. Associated with the tongue however, are specialized glands which have a separate purpose. Known as Von Ebner's Glands, or serous fluid producing minor salivary glands, this glandular epithelial tissue is specialized to hydrolize lipids found in vallate and foliate papillae [11]. Von Ebner's glands produce and secrete a fluid (much more watery than mucous) which contains enzymes called lingual lipases [11]. These are the enzymes responsible for one of the very first step in digestion, as they begin to break down lipid molecules. Von Ebner's glands are also thought to aid in taste perception as the fluid washes away any remaining chemical stimuli and creates an environment where a new stimuli can enter [11]. This means that these secretions are likely the reason that humans can respond to quickly changing stimuli.| Figure 10: Von Ebner's Glands |
Muscular Tissue
The muscles in the tongue are skeletal muscles that fall into multiple different planes, which allow the tongue to be capable of many unique and specific movements. In general the tongues skeletal muscles fall under two categories: Intrinsic and Extrinsic [1]. There are 4 main muscles of each category, for a total of 8 large muscles in the tongue.Intrinsic muscles are the muscles responsible for delicate movements and specific movements [1]. This means that these muscles are mainly active when the tongue needs to be moved in a precise manor, such as during speech. The four main intrinsic muscles are as follows:
| Figure 11: Intrinsic Muscles of the Human Tongue |
- Inferior Longitudinal Muscle: spans the length of the tongue (longitudinally) and is responsible for moving the apex of the tongue, and responsible for some shortening of the tongue [1].
- Superior Longitudinal Muscle: Spans the length of the tongue and is responsible for moving the apex in cooperation with the inferior longitudinal muscle [1].
- Transverse Muscle: Spans across the tongue and is responsible for narrowing the tongue [1].
- Vertical Muscle: Spans from the dorsal to ventral surface of the tongue and is responsible for flattening the tongue [1].
| Figure 12: Extrinsic Muscles of the Human Tongue |
- Hyoglossus: Connects the hyoid bone to the tongue and is responsible for retracting and depressing the tongue [1].
- Palatoglossus: Connects the palate to the tongue and is responsible for pulling the tongue back to its groove [1].
- Styloglossus: Connects the styloid process (behind the ear) to the tongue and is responsible for pulling the tongue upwards and towards the esophagus [1].
- Genioglossus: Connects the chin to the tongue and is responsible for sticking the tongue out and pulling it back. This muscle is also responsible for "troughing" the tongue [1].
The Taste Buds
| Figure 13: Light Microscope image of Taste Buds |
Structure
Taste buds are specialized receptor clusters which appear in the epithelial layer of some papillae in the tongue in terrestrial animals, but also appear on the lips, flanks and caudal fins of some fish species [9]. A papillae which contains taste buds is commonly referred to as a taste papillae. There are approximately 2,000-8,000 taste buds in the human tongue, although immense variation is seen between individuals [9].Taste buds are unlike many other receptor structures as they are mainly derived from precursor cells which are part of the epithelium [2]. Most other receptors in the human body are derived from nervous tissue, which has sparked some interest in taste receptor cells and their development. Further studies have confirmed that the majority of taste bud cells originate from the epithelium, although recent research has suggested a strong link between taste bud development and neural crest cells [2]. There has also been evidence to suggest a precursor which is apparent in the underlying connective tissue cells [2].
The traditional view of a taste bud was that it was a collection of 50-150 taste receptor cells which cluster together [9]. These taste buds have microvilli on their apical surface which reach out through small taste pores. The microvilli are covered in mucus, which brings chemical stimuli to the microvilli where they are sensed [9]. The signal is then sent through the cell and attaches to a neuron on the basal surface.
| Figure 14: Traditional View of Taste Bud Structure |
| Figure 15: Modern Proposed View of Taste Bud Structure |
Function
| Figure 16: Biochemical functioning of the Taste Bud Receptors |
The receptors on a taste cell are what respond differently to various chemicals, and produce different "flavours". These receptors work much like neurons receiving a neurotransmitter signal. When the tastant stimulates the receptor, it causes opening of a channel (ionotropic) or changes in the cells metabolism through G-protein manipulation (metabotropic) [10].
Different receptors exist for the 5 main flavours we know today; salty, sweet, sour, bitter and umami.
| Figure 17: Mammalian Taste Receptor Structures |
- Salty Receptors: epithelial-type sodium channel, which responds to different concentrations of sodium ions in the environment. Protons also may use these channels, explaining why eating acidic food reduces the saltiness of others [10].
- Sweet and Sour Receptors: these involve activation of G-protein linked receptors. Different pathways are used for specific sweeteners, which is how natural and artificial sweeteners may taste different [10].
- Bitter Receptors: Bitter tastants come in many classes (alkaloids, amino acids, urea, and some salts). These each use different receptors and pathways usually involving a specific G-protein called gustducin. If gustducin is non-functioning, bitter flavours will not be apparent [10].
- Umami Receptors: The umami flavour has only been recently discovered and has not been researched in much detail. It is thought to be a response to certain amino acids (specifically glutamate) which produce a savoury flavour. There are though to be many different pathways for umami [10].
The Tongue and Taste Buds Pathology
The tongue and taste buds have many diseases, ranging from bacterial and fungal infections, to general defects in their receptors. The following diseases are common in the tongue, but many are harmless to humans. WARNING: some of the pictures associated with the diseases will be gross, continue if you wish.Thrush (cadidiasis): Caused by a yeast (Candida albican) which grows over the surfaces of the oral cavity, including the tongue [5]. Thrush usually occurs in individuals with suppressed immune systems, although it can occur in anyone. Thrush can be treated using topical anti-fungal treatments or systemic oral azoles [3].
 |
| Figure 18: Candidiasis |
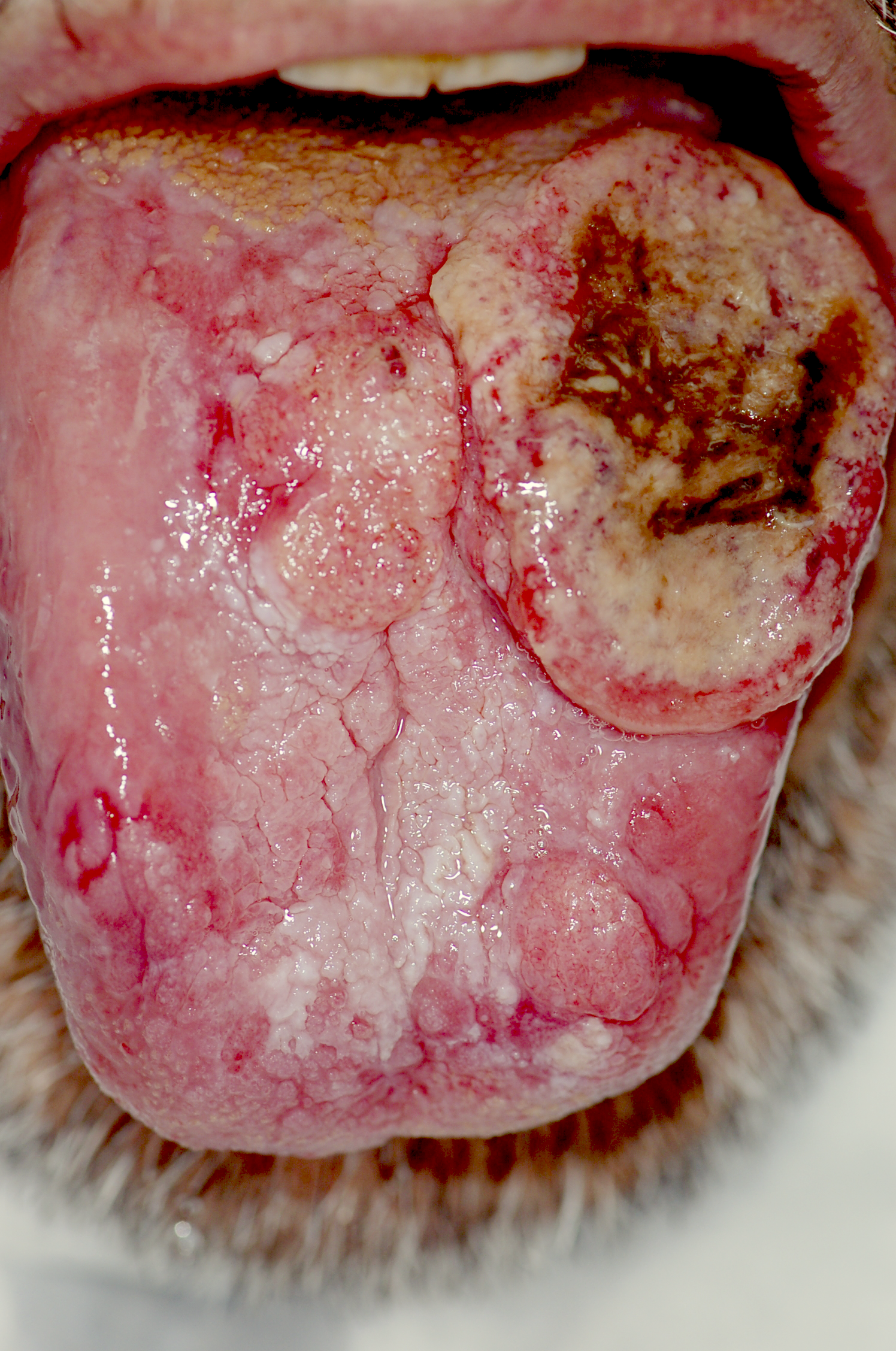 |
| Figure 19: Oral Cancer |
Macroglossia: This disease is also known as "big tongue". Macroglossia is exactly what it sounds like, it is a swelling or overgrowth of the tongue [5]. It can be caused during development by congenital defects, or later in life by inflammatory, traumatic, cancerous and metabolic causes [5].
| Figure 20: Macroglossia |
Geographic Tongue: This disease is named so because of the geographic appearance of tongues with this condition. The tongue appears cracked with ridges and coloured spots which move across the tongue's surface. Geographic tongue is typically harmless and is mainly caused by dehydration (can be mild, as in "dry mouth" in the morning) [5].
| Figure 21: Geographic Tongue |
Burning tongue: This is a syndrome in which there is a constant or erratic feeling of the burning or scalding of the tongue. This can be a symptom of underlying nerve damage, but is usually not the disease itself and is rarely treated alone [5].
 |
| Figure 22: Burning Tongue Syndrome |
Atrophic Glossitis: This disease is also called "bald tongue", because of the naked appearance of the tongue. The normal ridges and texture caused by the papillae disappear, as the papillae themselves lose their structure. This is commonly associated with a vitamin B deficiency and is also seen in anemic patients [5].
| Figure 23: Atrophic Glossitis (Bald Tongue) |
Hairy Tongue: This condition is almost the exact opposite of bald tongue. The papillae on the tongues surface can overgrow, creating an extremely ridged looking tongue, almost appearing hairy [5]. The treatment for this is usually to physically scrape off the excess papillae [5].
| Figure 24: Hairy Tongue |
Ageusia/Dysguesia: Dysguesia is a reduction in the ability to taste, whereas Ageusia is the complete loss of gustatory sensation altogether [6]. Ageusia is typically not associated with the taste buds themselves, but rather the other senses which determine flavour, specifically olfaction [6]. Non-olfactory ageusia can occur through damage to the taste buds or the nerves which transmit the signals from the tongue to the brain. Non-olfactory ageusia can be caused by local (oral infection, dentures, radiation), systemic (cancer, renal failure, liver failure), or neurological (Bell palsy, MS, viral infection) factors [6]. Ear damage can actually cause ageusia as it can potentially damage the chorda tympanii [6]. Hypoguesia also exists where taste perception is greatly increased [6].
References
[1]
Articulation: The Tongue. (n.d.). Retrieved October 18, 2016, from http://www.yorku.ca/earmstro/journey/tongue.html
[2]
Boggs, K., Venkatesan, N., Mederacke, I., Komatsu, Y., Stice, S., Schwabe, R.,
. . . Liu, H. (2016, January 7). Contribution of Underlying Connective Tissue
Cells to Taste Buds in Mouse Tongue and Soft Palate. PLoS One, 11(1).
[3]
Candidiasis Treatment & Management - Medscape Reference. (2016, October 6).
Retrieved October 18, 2016, from http://emedicine.medscape.com/article/213853-treatment
[4] Hill,
M. A. (2016). Tongue Development - Embryology. Retrieved October 18, 2016, from
https://embryology.med.unsw.edu.au/embryology/index.php/Tongue_Development
[5]
Hoffman, M. (n.d.). The Tongue (Human Anatomy). Retrieved October 18, 2016,
from http://www.webmd.com/oral-health/picture-of-the-tongue#1
[6]
Kieliszak, C., Peterson, A., & Joshi, A. (n.d.). Ageusia | 5-Minute Clinical
Consult - Unbound Medicine. Retrieved October 18, 2016, from http://www.unboundmedicine.com/5minute/view/5-Minute-Clinical-Consult/816154/all/Ageusia
[7] Oral
Mucosa | myVMC. (2015, May 14). Retrieved October 18, 2016, from http://www.myvmc.com/anatomy/oral-mucosa/
[8]
Peckham, M. (n.d.). Tongue Oral Tissue: Papillae of the Tongue Anterior Surface
of the Tongue. Retrieved October 18, 2016, from http://www.histology.leeds.ac.uk/oral/tongue.php
[9] Taste
Buds. (n.d.). Retrieved October 10, 2016, from https://www.britannica.com/science/taste-bud
[10]
Taste Receptors and the Transduction of Taste Signals ... (n.d.). Retrieved
October 10, 2016, from https://www.ncbi.nlm.nih.gov/books/NBK11148/
[11]
Varun. (n.d.). Minor Salivary Glands Types, Locations, and Functions. Retrieved
October 18, 2016, from http://www.juniordentist.com/minor-salivary-glands-types-location-and-function.html